Fight the Stigma
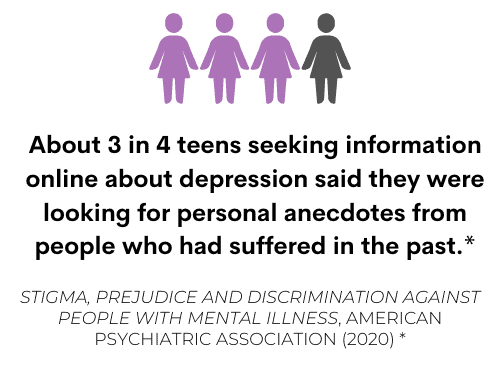
Why is it important to talk about mental health? We talk about many things that impact our society, but it is rare to have in-depth conversations about mental health even when it appears to be a buzzing topic. There are many stigmas attached to mental illness that may make it harder for someone experiencing mental struggles to reach out for help. Stigmas are negative beliefs of a group of people or a societal perception.
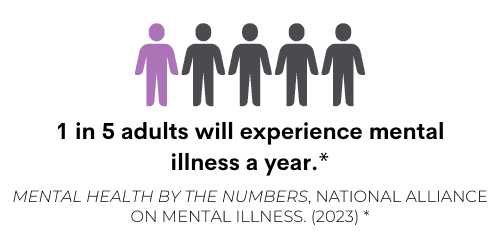
Stigmas can come in many forms, whether it is the language we use to describe someone, or things we see and read about people with mental illness. One example is the movie Joker (2019), where we see the protagonist become violent due to mental illness. Media may sometimes perpetuate common stigmas.
Stigmas can have harmful effects, like bullying or physical violence, difficulties at school or work, reluctance to seek help, lack of understanding from loved ones, and lack of hope.
There are many ways to address stigmas. This month we challenge you to:
- Talk openly about mental health, facts, and experiences
- Be conscious of language
- Say “Thank you for opening up to me” instead of “just deal with it!”
- Be honest about treatment
- Show compassion
Protective Factors
When people talk about what can be done regarding mental health, many professionals bring up protective factors. Protective factors are attributes that are linked or associated to healthy adjustment when facing adversity… basically they help us bounce back when we face trauma or hardships, which can also be known as resiliency. Protective factors can act like barriers against situations that we can’t control. We tend to ask why people experience certain illnesses and the most common reasons are genetics, environment, medical conditions, and life events.
While there are many different protective factors depending on your age or gender, there are a few that help everyone through many experiences.
Community support and social support are two of the biggest protective factors a person can have. Some protective factors include community gatherings, school, sports, employment, religion, and culture.
Another protective factor is words of affirmation, either to yourself or from others. A great way to visualize how protective factors impact us is to visualize ourselves as either an egg or tennis ball. In times of stress, the egg will inevitably crack while the tennis ball will continue to bounce back.
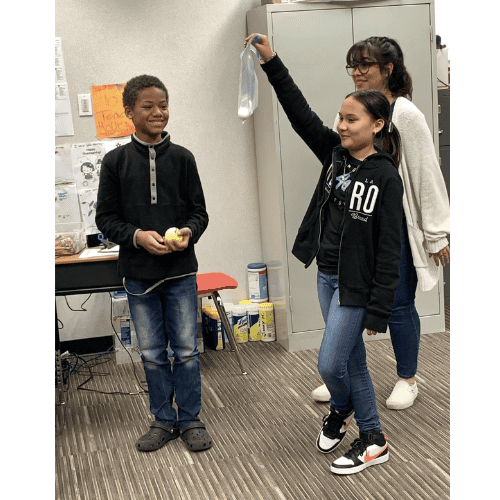
So, maybe you’re just dealing with a bad day and not a mental illness, the resiliency that comes from protective factors still helps you be like the tennis ball.
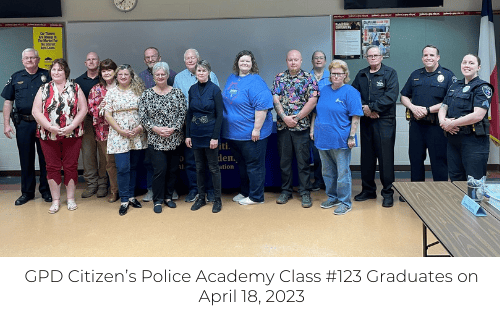
Police Week
In recognition of Mental Health Awareness Month and National Police Week, the CAPE team is spotlighting one of our local community partners, Gainesville Police Department (GPD), to discuss the topic of mental health. Police Officers are first responders to mental health crises, and a recent study from the American Psychological Association estimates that 20% of police calls involve a mental health crisis.* Our CAPE Team Director, Jennifer Burrows, sat down with Sgt. Cagle and Officer Mulkey to gain insight into GPD’s system for mental health crises and learn how officers are supported in their mental health as well. GPD currently has 5-6 patrol officers who are trained mental health peace officers, including Sgt. Cagle and Officer Mulkey. Officers are trained by the Texoma Community Center and learn about DSM* diagnosis and specific tools to reach someone in a crisis. “We have regular annual trainings that teach us simple stuff; to say their name frequently, make sure they know that you’re talking to them and it’s not the voices, but it also goes more in depth,” states Sgt. Cagle.

Officers are in contact with citizens needing care for mental health regularly and see them suffering due to no insurance. Citizens often aren’t able to get the care and support they need for a healthier life and both Sgt. Cagle and Officer Mulkey agree it’s sad to see populations of the community struggling. Sgt. Cagle mentioned, “I don’t think one shift goes by that we don’t see somebody that we know that has a mental health issue or we got called to them or we see them on the street…”
*DSM-Diagnostic and Statistical Manual of Mental Disorders
Spotlight and Events
Handling mental health crises as frequently as police do can take a toll on the mental health of the officer and their families. In addition to the frequent training for officers to handle mental health crises, GPD also participates in a peer program called “Texas Law Enforcement Peer Network.” “Peer to peer is an app for any police officer in the state of Texas. Our job is to listen… We don’t get into psychology or counseling or anything like that necessarily. We’re just a place to vent and offer resources [to other police officers],” shares Officer Mulkey. For clinical counseling needs, GPD has access to an Employee Assistance Program (EAP). “EAP provides assessment, short-term counseling, referral, management consultation, and coaching services to employees, and is available 24 hours a day, 365 days a year”.*
“Let’s say there’s an officer who’s deteriorating, we suspect something, maybe they’re posting stuff to Facebook, our supervisors can mandate them to go to EAP” shares Sgt. Cagle. All in all, it seems GPD is well equipped to handle mental health situations for both our citizens and officers and that is comforting to know as we raise awareness this month and say thanks to our police for all they do!
*Abramson, A. (2021). Building mental health into emergency responses.
Center, P. S. (2022). Employee Assistance Program (EAP). HHS.gov.
Center, P. S. (2022). Employee Assistance Program (EAP). HHS.gov.https://www.hhs.gov/about/agencies/asa/foh/bhs/employee-assistant-program/index.html